Navigating the complexities of mental health can be challenging, particularly when attempting to understand the subtle differences between various conditions. This guide offers a practical approach to identifying six common mental health conditions, emphasizing the importance of accurate diagnosis for effective treatment. We will explore key symptoms, diagnostic tools, and strategies for differentiating between similar conditions, ultimately empowering you with a clearer understanding of this crucial aspect of healthcare.
Understanding the nuances of mental health conditions requires a multifaceted approach. This guide will equip you with the knowledge to recognize the core symptoms of these conditions, understand how symptoms might overlap, and appreciate the role of diagnostic tools in arriving at an accurate diagnosis. We’ll delve into the process of clinical interviews and assessments, highlighting the critical role of a comprehensive evaluation in avoiding misdiagnosis and ensuring appropriate treatment.
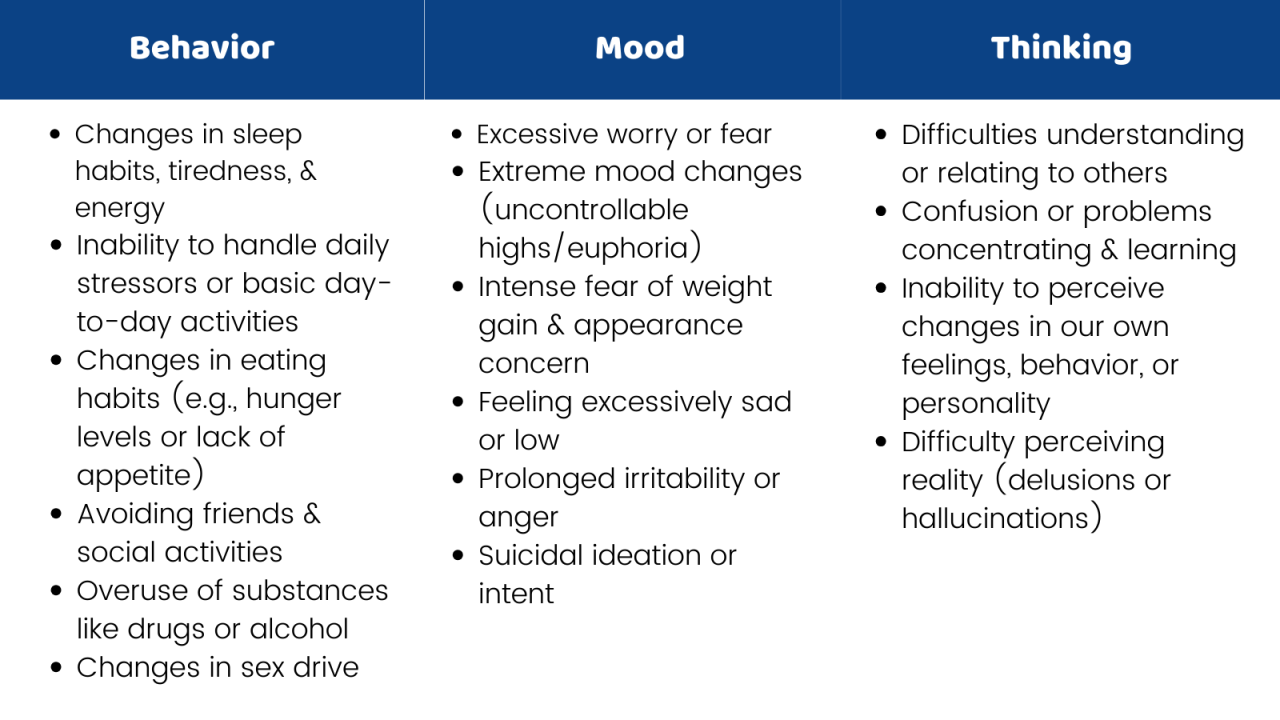
Understanding the Symptoms

Accurately diagnosing mental health conditions requires a thorough understanding of their diverse and often overlapping symptoms. While symptom presentation varies significantly between individuals, recognizing core patterns is crucial for appropriate treatment and support. This section details the common manifestations of six prevalent mental health conditions, emphasizing the complexities of differential diagnosis.
Common Manifestations of Six Mental Health Conditions
| Condition | Core Symptoms | Associated Symptoms | Severity Indicators |
|---|---|---|---|
| Major Depressive Disorder (MDD) | Persistent sadness, loss of interest or pleasure (anhedonia), fatigue, sleep disturbances (insomnia or hypersomnia). | Changes in appetite or weight, feelings of worthlessness or guilt, difficulty concentrating, thoughts of death or suicide. | Duration and intensity of symptoms, functional impairment (impact on work, relationships, daily activities), suicidal ideation. |
| Generalized Anxiety Disorder (GAD) | Excessive worry and anxiety about various events or activities, restlessness, difficulty concentrating, irritability. | Muscle tension, sleep disturbances, fatigue, difficulty controlling worry. | Frequency and intensity of worry, level of impairment in daily life, presence of physical symptoms. |
| Panic Disorder | Recurrent, unexpected panic attacks characterized by intense fear and physical symptoms. | Fear of future panic attacks (anticipatory anxiety), avoidance of situations associated with panic attacks, agoraphobia (fear of open spaces or public places). | Frequency and severity of panic attacks, degree of functional impairment due to avoidance behaviors. |
| Obsessive-Compulsive Disorder (OCD) | Obsessions (recurrent, intrusive thoughts, images, or urges) and compulsions (repetitive behaviors or mental acts performed to reduce anxiety). | Significant distress or impairment in social, occupational, or other important areas of functioning. | Time spent on obsessions and compulsions, level of distress caused by symptoms, impact on daily life. |
| Post-Traumatic Stress Disorder (PTSD) | Intrusive memories of a traumatic event, avoidance of reminders of the trauma, negative alterations in cognitions and mood, marked alterations in arousal and reactivity. | Irritability, outbursts of anger, difficulty sleeping, hypervigilance, exaggerated startle response. | Frequency and intensity of intrusive memories and avoidance behaviors, severity of negative alterations in mood and cognition, impact on daily life. |
| Social Anxiety Disorder (SAD) | Persistent fear of social situations where one might be scrutinized or embarrassed. | Avoidance of social situations, physical symptoms (e.g., blushing, sweating, trembling) during social interactions, self-consciousness. | Extent of avoidance behaviors, level of distress experienced in social situations, impact on social and occupational functioning. |
Symptom Overlap and Diagnostic Challenges
The symptoms listed above often overlap, making accurate diagnosis challenging. For instance, both depression and anxiety can present with fatigue, sleep disturbances, and difficulty concentrating. Similarly, symptoms of PTSD, such as irritability and sleep problems, can mimic those of other conditions. A comprehensive assessment considering the individual’s history, symptom duration, and the specific context of their experiences is crucial to differentiate between these conditions.
Comparative Symptom Profiles: MDD and GAD
Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD) share some overlapping symptoms, such as fatigue and sleep disturbances. However, a key difference lies in the predominant emotional experience. MDD is characterized by persistent sadness and loss of interest, while GAD is defined by excessive worry and anxiety about various aspects of life. Individuals with MDD may experience periods of low energy and motivation, while those with GAD may exhibit restlessness and difficulty relaxing. While both conditions can impact daily functioning, the nature of that impairment differs: MDD often leads to withdrawal and decreased productivity, whereas GAD can manifest as difficulty focusing, making decisions, or completing tasks. Accurate diagnosis requires careful consideration of these nuanced differences in symptom presentation.
Diagnostic Tools and Methods
Accurately diagnosing mental health conditions requires a multifaceted approach that combines various tools and methods. Healthcare professionals utilize a combination of clinical interviews, standardized assessments, and consideration of the individual’s history to arrive at a comprehensive diagnosis. This process aims to differentiate between similar conditions and ensure the most appropriate treatment plan is developed.
The Diagnostic Process: A Flowchart
A typical diagnostic process follows a series of steps. Imagine a flowchart beginning with a patient presenting with symptoms. The first step involves a comprehensive clinical interview to gather information about the patient’s history, current symptoms, and overall functioning. This interview guides the selection of appropriate standardized assessments. Based on the results of these assessments and the clinical interview, a provisional diagnosis is formulated. This diagnosis is then refined through further investigation, potentially including additional assessments or consultations with other specialists. Finally, a definitive diagnosis is reached, and a treatment plan is collaboratively developed with the patient. The flowchart would visually represent this sequential process with decision points based on the information gathered at each stage. For example, if the initial interview suggests symptoms consistent with depression, the next step would be to administer a depression-specific assessment. If the assessment results fall within a certain range, a diagnosis of depression may be considered. However, if the results are inconclusive or suggest other conditions, further investigation would be necessary.
Standardized Questionnaires and Assessments
Standardized questionnaires and assessments, such as those aligned with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, play a crucial role in the diagnostic process. These tools provide structured methods for evaluating symptoms and severity, allowing for more objective and reliable diagnoses. For example, the Patient Health Questionnaire-9 (PHQ-9) is a widely used questionnaire for assessing the severity of depressive symptoms, while the Generalized Anxiety Disorder 7-item scale (GAD-7) is used for anxiety. These assessments provide quantifiable data that helps clinicians differentiate between conditions and monitor treatment progress. The DSM-5 itself provides detailed criteria for each mental health disorder, serving as a guide for clinicians in making accurate diagnoses. Using these standardized tools enhances the consistency and reliability of diagnoses across different clinicians and settings.
Clinical Interviews and Relevant Questions
Clinical interviews are essential for gathering detailed information about a patient’s history, current symptoms, and functioning. These interviews are open-ended and allow for a flexible exploration of the patient’s experience. Examples of questions used in clinical interviews might include: “Can you describe your current mood?”, “How long have you been experiencing these symptoms?”, “How are these symptoms impacting your daily life?”, “Have you experienced any similar episodes in the past?”, “Is there anything that seems to trigger or worsen your symptoms?”, and “What coping mechanisms have you tried?”. The answers to these questions provide valuable contextual information that helps to understand the nature and severity of the symptoms and formulate a diagnosis. The interview also provides an opportunity to build rapport and establish a therapeutic alliance with the patient.
Red Flags Requiring Immediate Professional Attention
Several red flags may indicate the need for immediate professional attention.
- Suicidal thoughts or ideation, including planning or attempts.
- Self-harm behaviors, such as cutting or burning.
- Severe anxiety or panic attacks that interfere with daily functioning.
- Psychotic symptoms, such as hallucinations or delusions.
- Sudden and significant changes in behavior or mood.
- Unexplained changes in physical health, such as significant weight loss or insomnia, that may be indicative of an underlying mental health condition.
These red flags necessitate prompt evaluation and intervention by a mental health professional to prevent potential harm. The presence of any of these signs warrants immediate attention and intervention to mitigate risks and ensure the safety and well-being of the individual.
Differentiating Between Conditions
Accurate diagnosis is paramount in mental healthcare. Misdiagnosis can lead to ineffective or even harmful treatment, delaying recovery and potentially worsening symptoms. A comprehensive evaluation, considering various factors beyond just reported symptoms, is crucial for differentiating between similar conditions and ensuring the most appropriate treatment plan.
A thorough evaluation typically involves a detailed clinical interview, psychological assessments, and sometimes, neurological or medical examinations to rule out other contributing factors. This multi-faceted approach helps clinicians build a complete picture of the individual’s mental state, enabling a more precise diagnosis.
Treatment Approaches and Diagnostic Influence
Treatment approaches vary significantly depending on the specific diagnosis. For example, someone diagnosed with Generalized Anxiety Disorder (GAD) might benefit from cognitive-behavioral therapy (CBT) and possibly medication like selective serotonin reuptake inhibitors (SSRIs). In contrast, someone with Major Depressive Disorder (MDD) might also receive CBT and SSRIs, but the focus of therapy and medication management might differ, concentrating on addressing depressive symptoms more directly. Similarly, treatment for Post-Traumatic Stress Disorder (PTSD) often involves trauma-focused therapy, such as prolonged exposure therapy or eye movement desensitization and reprocessing (EMDR), alongside potential medication for associated symptoms like anxiety or sleep disturbances. The distinct symptom profiles and underlying mechanisms of each condition necessitate tailored interventions. Misdiagnosis can lead to a treatment plan that doesn’t address the core issues, resulting in limited or no improvement.
Potential Biases and Factors Affecting Diagnostic Accuracy
Several factors can influence diagnostic accuracy. Cultural biases, where a clinician’s understanding of cultural norms might misinterpret certain behaviors or symptoms, are a significant concern. For instance, expressions of grief or distress might be misinterpreted as signs of a mental illness in some cultures, leading to unnecessary diagnosis. Clinician bias, where personal beliefs or experiences might unconsciously influence their assessment, is another potential issue. Furthermore, the severity and presentation of symptoms can vary greatly between individuals, making diagnosis challenging. A patient’s willingness to disclose information, influenced by factors like stigma or trust in the clinician, also plays a crucial role.
Strategies for mitigating these biases include ongoing professional development focusing on cultural competency and implicit bias awareness training for clinicians. Structured diagnostic interviews and standardized assessment tools can help reduce subjectivity. Encouraging open communication and building rapport with the patient fosters trust and increases the likelihood of accurate reporting of symptoms.
Conditions Frequently Confused
The following table highlights some conditions that can be easily confused, emphasizing key distinguishing features to aid in accurate diagnosis.
| Condition | Key Distinguishing Features |
|---|---|
| Major Depressive Disorder (MDD) | Persistent low mood, loss of interest, changes in sleep and appetite, feelings of worthlessness or guilt. Symptoms typically last for at least two weeks. |
| Persistent Depressive Disorder (Dysthymia) | Similar to MDD but symptoms are less severe but more chronic, lasting at least two years. |
| Generalized Anxiety Disorder (GAD) | Excessive worry and anxiety about various aspects of life, often accompanied by physical symptoms like restlessness, fatigue, and difficulty concentrating. |
| Panic Disorder | Characterized by recurrent, unexpected panic attacks, intense fear and discomfort, with physical symptoms like rapid heartbeat, shortness of breath, and dizziness. |
| Obsessive-Compulsive Disorder (OCD) | Presence of obsessions (recurring intrusive thoughts) and compulsions (repetitive behaviors or mental acts) aimed at reducing anxiety associated with obsessions. |
| Post-Traumatic Stress Disorder (PTSD) | Develops after experiencing or witnessing a traumatic event, characterized by intrusive memories, flashbacks, avoidance of reminders of the trauma, and heightened arousal. |
Conclusion

Accurately diagnosing mental health conditions is paramount for effective treatment and improved patient outcomes. By understanding the core symptoms, utilizing appropriate diagnostic tools, and recognizing the potential for overlapping symptoms, healthcare professionals and individuals alike can navigate the complexities of mental health with increased confidence. This guide has provided a framework for recognizing common conditions, differentiating between them, and ultimately, fostering a more informed approach to mental well-being.