Understanding the intricacies of eye health is crucial for maintaining clear vision and overall well-being. This exploration delves into the diagnosis of eight common eye conditions, providing a comprehensive overview of symptoms, diagnostic procedures, and treatment considerations. From initial symptom assessment to advanced diagnostic techniques, we will navigate the complexities of identifying and managing these conditions, emphasizing the importance of accurate diagnosis to prevent potential complications.
We will examine a range of conditions, highlighting the nuances of each and the importance of differentiating between similar presentations. The diagnostic pathways explored will incorporate both common symptoms and advanced procedures, providing a practical guide for healthcare professionals and a valuable resource for individuals seeking to understand their eye health better. Accurate and timely diagnosis is paramount in preserving visual acuity and preventing long-term damage.
Common Symptoms and Initial Diagnosis
Accurate and timely diagnosis of eye conditions is crucial for effective treatment and preventing vision loss. Understanding common symptoms and employing a systematic diagnostic approach are key steps in this process. This section details the typical symptoms associated with eight common eye conditions, provides a diagnostic flowchart, and offers a comparative table highlighting key differentiating features.
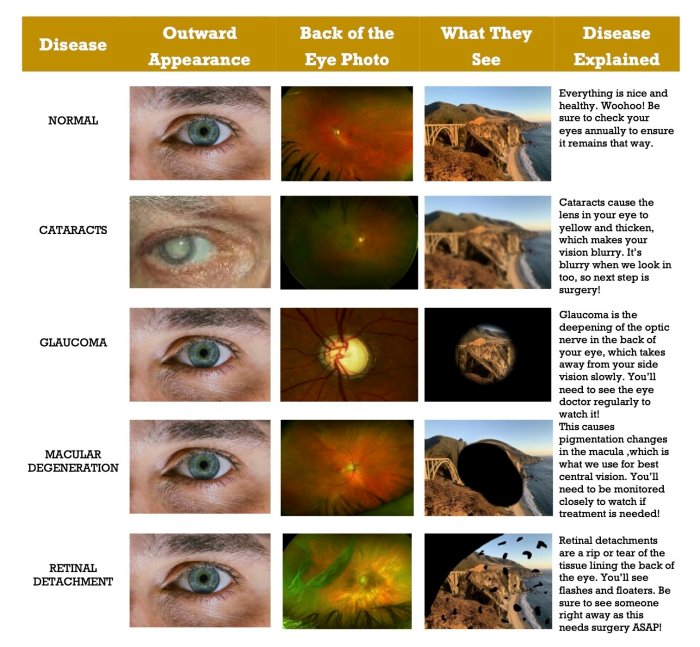
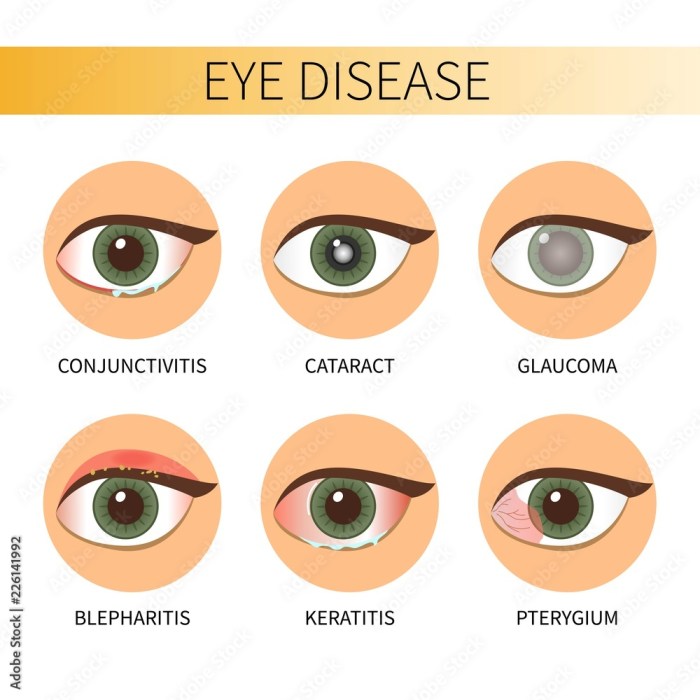
Typical Symptoms of Eight Eye Conditions
The symptoms of various eye conditions can overlap, making accurate diagnosis challenging. However, certain symptoms are more indicative of specific conditions. Careful observation and a detailed patient history are vital.
Diagnostic Flowchart for Initial Eye Problem Assessment
The following flowchart Artikels a logical pathway for the initial assessment of eye problems. It guides the clinician through a series of questions and observations to narrow down the possibilities.
[Diagram description: The flowchart would begin with a central box labeled “Patient Presents with Eye Problem.” This would branch into two boxes: “Visual Acuity Affected?” (Yes/No). A “Yes” branch would lead to a series of boxes addressing blurry vision (near/far), floaters, flashes, etc., each leading to possible diagnoses. A “No” branch would address pain, redness, discharge, etc., leading to other diagnoses. Each diagnostic possibility would have a box indicating further investigation required.]
Comparative Table of Initial Symptoms
The following table compares and contrasts the initial symptoms of eight common eye conditions. Note that these are not exhaustive lists, and some conditions may present with atypical symptoms.
| Condition | Primary Symptom | Secondary Symptom | Possible Differential Diagnoses |
|---|---|---|---|
| Dry Eye Disease | Burning, itching, gritty sensation | Redness, blurry vision, excessive tearing (paradoxical) | Blepharitis, corneal abrasion |
| Conjunctivitis (Pink Eye) | Redness, itching, discharge | Swollen eyelids, light sensitivity | Allergic conjunctivitis, bacterial conjunctivitis, viral conjunctivitis |
| Glaucoma | Gradual vision loss (peripheral initially) | Halos around lights, eye pain (in acute cases) | Cataracts, macular degeneration |
| Cataracts | Blurry vision, cloudy vision | Glare sensitivity, faded colors | Macular degeneration, glaucoma |
| Macular Degeneration | Central vision loss, blurred vision | Distorted vision, blind spots | Glaucoma, cataracts, diabetic retinopathy |
| Diabetic Retinopathy | Blurry vision, floaters | Blind spots, vision loss | Macular degeneration, glaucoma |
| Blepharitis | Red, inflamed eyelids | Itching, burning, crusting | Dry eye disease, conjunctivitis |
| Corneal Abrasion | Severe eye pain, blurry vision | Photophobia (light sensitivity), tearing | Foreign body in eye, corneal ulcer |
Advanced Diagnostic Procedures
Following initial assessment of common symptoms, several advanced diagnostic procedures are employed to confirm the diagnosis and determine the severity of various eye conditions. These procedures provide detailed anatomical and functional information, guiding appropriate treatment strategies. The selection of procedures depends on the suspected condition and the information needed to formulate a comprehensive treatment plan.
Advanced Diagnostic Procedures for Refractive Errors (Myopia, Hyperopia, Astigmatism)
Refractive errors, including myopia, hyperopia, and astigmatism, are primarily diagnosed using automated phoropters and retinoscopy. However, advanced techniques provide more precise measurements crucial for complex cases or refractive surgery. These include keratometry (measuring corneal curvature), which uses a keratometer to assess the shape of the cornea, and optical coherence tomography (OCT), which provides high-resolution images of the cornea and anterior segment. Interpretation of results involves comparing measured refractive errors with visual acuity to determine the degree of correction needed. For example, a high degree of myopia might be indicated by a significantly elongated eyeball detected through OCT imaging and a correspondingly low visual acuity.
Advanced Diagnostic Procedures for Cataracts
Cataract diagnosis typically begins with a visual acuity test and a slit-lamp examination. Advanced diagnostic tools enhance the assessment of cataract severity and surgical planning. These include biometry (measuring the length of the eye to determine the power of an intraocular lens implant), which uses ultrasound to measure the axial length of the eye, and optical coherence tomography (OCT), which allows detailed visualization of the lens and surrounding structures. Interpretation involves assessing the density and location of opacities within the lens, with denser opacities and greater extent of opacification indicating more advanced cataracts. For example, an OCT image clearly showing significant lens opacification and disruption of the lens structure would indicate the need for cataract surgery.
Advanced Diagnostic Procedures for Glaucoma
Glaucoma diagnosis relies on measuring intraocular pressure (IOP) and assessing the optic nerve head. Advanced diagnostic procedures provide a more comprehensive evaluation of glaucoma progression. These include gonioscopy (examining the angle where the iris meets the cornea), which uses a special lens to visualize the drainage angle of the eye, and optical coherence tomography (OCT), which provides high-resolution images of the optic nerve head and retinal nerve fiber layer. Interpretation focuses on identifying characteristic changes in the optic nerve head, such as cupping, and thinning of the retinal nerve fiber layer, as well as assessing the IOP and the angle of the eye. For example, a significant reduction in retinal nerve fiber layer thickness detected by OCT, coupled with elevated IOP and narrowed drainage angle detected by gonioscopy, strongly suggests glaucoma.
Advanced Diagnostic Procedures for Macular Degeneration
Early detection of macular degeneration often relies on visual acuity tests and Amsler grid testing. Advanced imaging techniques are essential for assessing disease severity and monitoring progression. These include fundus photography (taking high-resolution images of the retina), which documents changes in the macula, and optical coherence tomography angiography (OCTA), which visualizes the retinal vasculature to detect subtle changes in blood flow. Interpretation involves identifying characteristic features of macular degeneration, such as drusen (yellow deposits under the retina) and neovascularization (abnormal blood vessel growth). For example, the presence of numerous large drusen and neovascularization detected by OCTA indicates a more advanced and potentially more aggressive form of macular degeneration.
Advanced Diagnostic Procedures for Diabetic Retinopathy
Diabetic retinopathy diagnosis initially involves a dilated eye exam. Advanced imaging is crucial for assessing the severity of retinal damage and guiding treatment. These include fluorescein angiography (injecting a dye to visualize retinal blood vessels), which highlights areas of leakage and abnormal blood vessel growth, and optical coherence tomography (OCT), which provides detailed images of the retinal layers and assesses the presence of macular edema. Interpretation involves identifying microaneurysms, hemorrhages, and neovascularization, with the extent and severity of these findings correlating with the severity of diabetic retinopathy. For instance, widespread neovascularization and significant macular edema detected by fluorescein angiography and OCT indicate a severe form of proliferative diabetic retinopathy.
Advanced Diagnostic Procedures for Dry Eye Disease
Dry eye disease is often diagnosed based on symptoms and a physical examination. Advanced diagnostic procedures provide objective measures of tear film function and ocular surface health. These include tear film breakup time (TBUT) measurement, which assesses the stability of the tear film, and Schirmer test, which measures tear production. In addition, osmolarity testing can quantify the tear film’s salt concentration, and corneal staining helps to evaluate the level of corneal damage. Interpretation of results focuses on identifying abnormalities in tear production, tear film stability, and ocular surface damage. For example, a reduced TBUT, decreased Schirmer test score, and elevated tear osmolarity would all point towards a diagnosis of dry eye disease.
Advanced Diagnostic Procedures for Age-Related Macular Degeneration (AMD)
AMD diagnosis often begins with visual acuity tests and Amsler grid testing. Advanced imaging techniques are vital for assessing the severity of macular damage and monitoring progression. These include fundus autofluorescence (FAF) imaging, which highlights areas of retinal pigment epithelium dysfunction, and optical coherence tomography (OCT), which provides high-resolution images of the retinal layers. Interpretation involves identifying characteristic features of AMD, such as drusen (yellow deposits under the retina) and geographic atrophy (loss of retinal tissue). For example, the presence of numerous large drusen and geographic atrophy detected by OCT and FAF would indicate an advanced stage of AMD.
Advanced Diagnostic Procedures for Retinal Detachment
Retinal detachment is typically diagnosed through a dilated eye examination. Advanced imaging techniques confirm the diagnosis and assess the extent of detachment. These include ultrasound biomicroscopy (UBM), which uses ultrasound waves to image the eye’s structures, and optical coherence tomography (OCT), which provides high-resolution images of the retinal layers. Interpretation focuses on identifying the location and extent of the retinal detachment. For example, UBM might show a detached retina as a hyporeflective area, while OCT would provide detailed visualization of the detached retinal layers and the subretinal fluid.
| Condition | Suitable Procedures | Less Suitable Procedures | Reasons for Suitability/Unsuitability |
|---|---|---|---|
| Refractive Errors | Keratometry, OCT | Fluorescein Angiography | Keratometry measures corneal curvature; OCT provides high-resolution images of the cornea; Fluorescein angiography is not relevant to refractive errors. |
| Cataracts | Biometry, OCT | Gonioscopy | Biometry measures eye length for IOL calculation; OCT visualizes lens structure; Gonioscopy examines the drainage angle, irrelevant to cataracts. |
| Glaucoma | Gonioscopy, OCT | Biometry | Gonioscopy visualizes drainage angle; OCT images optic nerve and retinal nerve fiber layer; Biometry is primarily used for cataract surgery planning. |
| Macular Degeneration | Fundus Photography, OCTA | Keratometry | Fundus photography documents retinal changes; OCTA visualizes retinal vasculature; Keratometry is for corneal curvature measurement. |
| Diabetic Retinopathy | Fluorescein Angiography, OCT | Keratometry | Fluorescein angiography visualizes retinal blood vessels; OCT assesses retinal layers; Keratometry is unrelated to diabetic retinopathy. |
| Dry Eye Disease | TBUT, Schirmer Test, Osmolarity Testing, Corneal Staining | Biometry | These tests assess tear film function and ocular surface health; Biometry is for lens implant power calculation. |
| Age-Related Macular Degeneration (AMD) | FAF, OCT | Gonioscopy | FAF highlights retinal pigment epithelium dysfunction; OCT images retinal layers; Gonioscopy is for assessing the drainage angle. |
| Retinal Detachment | UBM, OCT | Schirmer Test | UBM uses ultrasound to image retinal detachment; OCT provides detailed visualization; Schirmer test measures tear production. |
Differential Diagnosis and Treatment Considerations

Accurate diagnosis is paramount in ophthalmology, as the diverse range of eye conditions often present with overlapping symptoms. Failing to consider differential diagnoses can lead to inappropriate treatment and potentially severe complications. A thorough evaluation, including a detailed patient history and comprehensive ophthalmological examination, is crucial to differentiate between similar conditions and ensure the correct treatment plan is implemented.
Differential Diagnosis Examples
Differentiating between various eye conditions requires careful consideration of the patient’s symptoms, medical history, and the results of diagnostic tests. For instance, blurred vision could stem from refractive errors (myopia, hyperopia, astigmatism), cataracts, macular degeneration, or diabetic retinopathy. Similarly, redness and pain could indicate conjunctivitis, corneal ulcer, uveitis, or even glaucoma. A thorough examination helps pinpoint the underlying cause. Consider a patient presenting with sudden vision loss. This could be caused by retinal detachment, central retinal artery occlusion, or even a stroke affecting the visual pathway. Each requires a vastly different treatment approach.
Treatment Comparisons and Contrasts
Treatments for the eight eye conditions vary widely depending on the specific condition and its severity. Refractive errors are typically corrected with eyeglasses, contact lenses, or refractive surgery. Cataracts often necessitate surgical removal and lens implantation. Glaucoma management usually involves medication to lower intraocular pressure, potentially supplemented by laser treatment or surgery. Macular degeneration treatments focus on slowing disease progression with medication or injections. Diabetic retinopathy treatment depends on the severity, ranging from lifestyle modifications and blood sugar control to laser photocoagulation or surgery. Dry eye disease management often includes artificial tears, lid hygiene, and in some cases, punctal plugs. Conjunctivitis treatment generally involves topical antibiotics or antivirals if an infection is identified. Corneal ulcers require prompt treatment with antibiotics or antifungals to prevent vision loss or perforation.
Potential Complications of Misdiagnosis or Delayed Treatment
The consequences of misdiagnosis or delayed treatment can be severe, potentially leading to permanent vision impairment or even blindness. The following lists illustrate the potential complications for each condition:
Refractive Errors
Delayed correction of refractive errors can lead to eye strain, headaches, and amblyopia (lazy eye) in children.
Cataracts
Delayed cataract surgery can result in significant vision loss, increased risk of glaucoma, and reduced quality of life.
Glaucoma
Untreated glaucoma leads to progressive vision loss, eventually resulting in blindness.
Macular Degeneration
Delayed or inadequate treatment can accelerate vision loss, impacting daily activities and independence.
Diabetic Retinopathy
Untreated diabetic retinopathy can cause severe vision loss, blindness, and retinal detachment.
Dry Eye Disease
Chronic dry eye can lead to corneal damage, scarring, and persistent discomfort.
Conjunctivitis
While usually self-limiting, untreated bacterial conjunctivitis can spread and cause complications.
Corneal Ulcers
Delayed treatment can result in corneal perforation, scarring, vision loss, and even loss of the eye.
Conclusion
Accurate diagnosis of eye conditions is pivotal for effective treatment and preserving vision. This comprehensive overview has highlighted the importance of considering a wide range of symptoms, utilizing appropriate diagnostic procedures, and carefully weighing differential diagnoses. By understanding the nuances of each condition and the potential complications of misdiagnosis, healthcare professionals can provide optimal care, leading to improved patient outcomes and a higher quality of life for those affected by eye diseases.