High blood pressure, a silent yet pervasive health concern, affects millions globally. Understanding its causes is crucial for effective management and prevention. This exploration delves into eight common contributors to hypertension, examining their physiological mechanisms, risk factors, and associated lifestyle choices. We’ll also detail diagnostic methods, emphasizing accuracy and the importance of regular blood pressure monitoring.
From the intricacies of kidney function to the impact of dietary habits, we will unravel the complexities of this widespread condition. This comprehensive guide aims to empower individuals with the knowledge to understand their risk, seek appropriate medical attention, and make informed choices to protect their cardiovascular health.
Understanding the Eight Common Causes of High Blood Pressure

High blood pressure, or hypertension, is a significant health concern affecting millions worldwide. Understanding its various causes is crucial for effective prevention and management. This section will explore eight common causes, detailing their physiological mechanisms, prevalence, risk factors, and lifestyle contributions.
Primary Hypertension (Essential Hypertension)
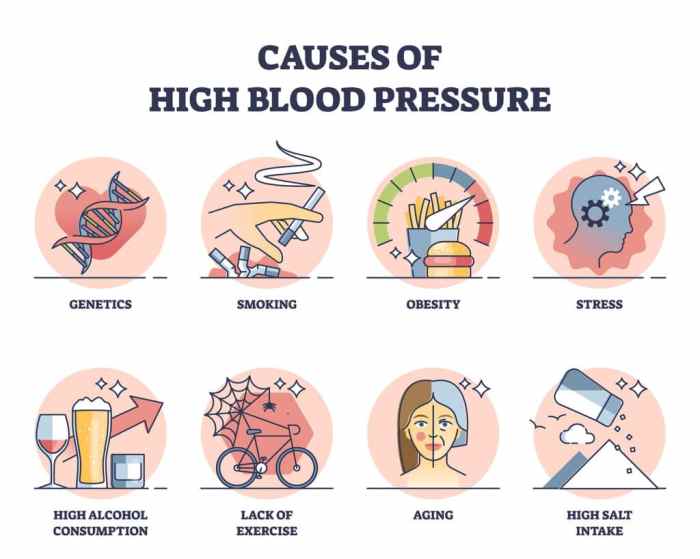
Primary hypertension accounts for the vast majority of high blood pressure cases. Its exact cause remains unknown, but it’s believed to be a complex interplay of genetic and environmental factors. Physiological mechanisms often involve dysfunction in the renin-angiotensin-aldosterone system (RAAS), leading to increased vascular resistance and sodium retention. Prevalence is high, especially in older adults, and risk factors include family history, obesity, and unhealthy diets high in sodium. Lifestyle choices such as excessive salt intake, lack of physical activity, and chronic stress significantly contribute to primary hypertension.
Secondary Hypertension
Unlike primary hypertension, secondary hypertension results from an identifiable underlying medical condition. Several diseases and conditions can elevate blood pressure, including kidney disease, obstructive sleep apnea, adrenal gland disorders (such as Cushing’s syndrome and pheochromocytoma), and certain medications. The physiological mechanisms vary depending on the underlying cause; for example, kidney disease can lead to increased renin production, while sleep apnea causes intermittent hypoxia, increasing vascular tone. Prevalence varies depending on the underlying condition, and risk factors are specific to each cause. Lifestyle factors play a role, but the primary focus is on managing the underlying condition.
Obesity
Obesity is a major contributor to high blood pressure. Excess body fat, particularly visceral fat (around the organs), increases resistance to insulin, leading to insulin resistance and increased inflammation. This, in turn, can damage blood vessels and raise blood pressure. The prevalence of obesity is rising globally, contributing to the increasing incidence of hypertension. Risk factors include poor diet, lack of physical activity, and genetic predisposition. Lifestyle choices like consuming a high-calorie, processed food diet and sedentary behavior significantly increase the risk.
Diabetes Mellitus
Diabetes mellitus, both type 1 and type 2, is strongly linked to hypertension. High blood sugar levels damage blood vessels, leading to increased vascular resistance and blood pressure. The chronic inflammation associated with diabetes also contributes. Prevalence is high, and risk factors include genetic predisposition, obesity, and lifestyle factors. Uncontrolled blood sugar levels and unhealthy lifestyle choices such as poor diet and lack of exercise exacerbate the risk of hypertension.
Chronic Kidney Disease
Chronic kidney disease (CKD) can cause high blood pressure through several mechanisms. Damaged kidneys may not effectively filter sodium and water, leading to fluid retention and increased blood volume. They also may produce excessive amounts of renin, further increasing blood pressure. Prevalence of CKD is increasing, and risk factors include diabetes, hypertension (itself), and glomerulonephritis. Lifestyle choices, while important for overall health, are less directly impactful than addressing the underlying kidney disease.
Alcohol Consumption
Excessive alcohol consumption raises blood pressure. Alcohol directly affects blood vessels, causing them to constrict and increasing blood pressure. It can also interfere with the body’s regulation of fluids and electrolytes. Prevalence of alcohol-related hypertension varies widely depending on cultural norms and individual consumption patterns. Risk factors include excessive alcohol intake and genetic predisposition to alcohol sensitivity. Moderation of alcohol consumption or abstinence is crucial.
Stress
Chronic stress can significantly elevate blood pressure. Stress hormones, such as adrenaline and cortisol, increase heart rate and constrict blood vessels, leading to temporary and potentially long-term increases in blood pressure. Prevalence of stress-related hypertension is high, particularly in individuals with stressful lifestyles or poor coping mechanisms. Risk factors include job stress, financial worries, and relationship problems. Lifestyle changes like stress management techniques (yoga, meditation) and regular exercise are vital.
Smoking
Smoking damages blood vessels and increases the risk of hypertension. Nicotine constricts blood vessels, increasing blood pressure, and other toxins in cigarette smoke promote inflammation and atherosclerosis. Prevalence of smoking-related hypertension is high among smokers. Risk factors include smoking habits and exposure to secondhand smoke. Quitting smoking is the most effective lifestyle change.
| Cause | Symptoms | Treatment | Long-Term Effects |
|---|---|---|---|
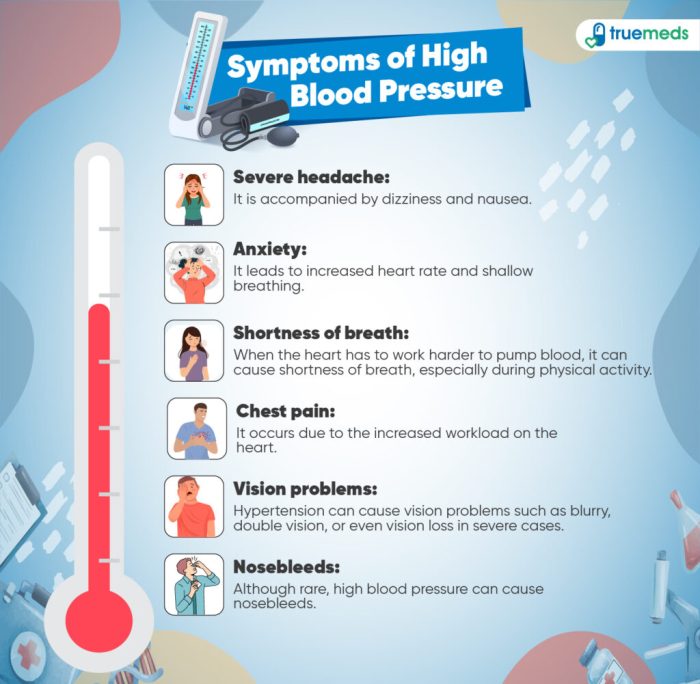
| Primary Hypertension | Often asymptomatic; headaches, dizziness, shortness of breath (in severe cases) | Lifestyle modifications, medication (ACE inhibitors, ARBs, diuretics, beta-blockers) | Stroke, heart attack, kidney failure, blindness |
| Secondary Hypertension | Symptoms vary depending on the underlying cause; may include those of the underlying condition | Treatment of the underlying condition; medication may be needed to control blood pressure | Depends on the underlying condition and its treatment; may include those of the underlying condition |
| Obesity | Often asymptomatic; may experience shortness of breath, fatigue | Weight loss through diet and exercise; medication may be needed | Increased risk of cardiovascular disease, type 2 diabetes, certain cancers |
| Diabetes Mellitus | Increased thirst, frequent urination, fatigue; may be asymptomatic | Blood sugar control; medication may be needed to control blood pressure | Increased risk of cardiovascular disease, kidney failure, blindness, nerve damage |
| Chronic Kidney Disease | Fatigue, swelling, shortness of breath; may be asymptomatic | Management of underlying kidney disease; medication may be needed to control blood pressure | Kidney failure, cardiovascular disease |
| Alcohol Consumption | Often asymptomatic; may experience headaches, flushing | Moderation or abstinence from alcohol; medication may be needed | Increased risk of cardiovascular disease, liver disease |
| Stress | Headaches, muscle tension, irritability, sleep disturbances | Stress management techniques (yoga, meditation); medication may be needed | Increased risk of cardiovascular disease, anxiety disorders |
| Smoking | Often asymptomatic; may experience shortness of breath | Smoking cessation; medication may be needed | Increased risk of cardiovascular disease, lung cancer, other cancers |
Diagnostic Methods for High Blood Pressure
Diagnosing high blood pressure, or hypertension, involves a combination of methods focusing on accurate blood pressure measurement and, in some cases, further investigations to identify underlying causes. Accurate measurement is crucial, as misdiagnosis can lead to unnecessary treatment or, conversely, delayed intervention in serious cases. This section details the processes involved in diagnosing hypertension.
Clinical Blood Pressure Measurement
A healthcare professional typically uses a sphygmomanometer and stethoscope to measure blood pressure. This involves inflating a cuff around the upper arm, listening for Korotkoff sounds (the sounds of blood flowing through the artery) with a stethoscope, and noting the systolic (highest) and diastolic (lowest) pressure readings. Accurate placement of the cuff is paramount; it should be positioned at heart level, snug but not too tight, with the lower edge approximately 2.5 cm above the antecubital fossa (the crease of the elbow). The patient should be seated comfortably, with their arm supported and relaxed, avoiding talking or movement during the measurement. Multiple readings should be taken, with at least a minute between each, to ensure accuracy.
Home Blood Pressure Monitoring
Home blood pressure monitoring provides a more comprehensive picture of blood pressure fluctuations throughout the day. Automatic devices are readily available and relatively easy to use. Accuracy depends on correct technique, which often includes ensuring the cuff fits properly and taking readings at the same time of day, following the manufacturer’s instructions carefully. Home monitoring allows for the detection of “white coat hypertension” (elevated readings in a clinical setting only) and “masked hypertension” (normal readings in a clinical setting but elevated readings at home). Consistent recording of readings and sharing them with a healthcare professional is essential for effective management.
Sources of Error in Blood Pressure Measurement and Mitigation Strategies
Several factors can influence blood pressure readings, leading to inaccurate results. These include improper cuff size (too small or too large), incorrect cuff placement, patient movement, talking during measurement, caffeine or nicotine consumption shortly before measurement, and a full bladder. To minimize errors, healthcare professionals should use appropriately sized cuffs, ensure proper cuff placement, instruct patients to remain still and quiet, and consider asking about recent caffeine or nicotine intake. For home monitoring, consistent technique and adherence to manufacturer instructions are crucial.
Steps in Diagnosing High Blood Pressure
The diagnostic process typically involves the following steps:
- Initial blood pressure measurement: The healthcare professional takes at least two readings, with a minute’s rest between them, using a properly sized cuff and correct technique.
- Confirmation of elevated readings: If the initial readings indicate hypertension, additional readings are taken on subsequent visits to confirm the diagnosis.
- Lifestyle assessment: The healthcare professional will inquire about the patient’s lifestyle, including diet, exercise habits, smoking status, alcohol consumption, and stress levels. This helps identify potential modifiable risk factors.
- Follow-up tests and referrals (if necessary): If hypertension is confirmed, further investigations might be ordered to rule out secondary causes (e.g., kidney disease, sleep apnea). This may include blood and urine tests, electrocardiogram (ECG), and potentially referral to a specialist such as a nephrologist or cardiologist.
Lifestyle Modifications and Treatment Options for High Blood Pressure

Managing high blood pressure, regardless of its underlying cause, often involves a combination of lifestyle changes and, in many cases, medication. The effectiveness of each approach varies depending on the individual, the severity of hypertension, and the presence of other health conditions. A holistic approach, integrating both lifestyle adjustments and medical interventions tailored to the specific cause, generally yields the best results.
Effectiveness of Lifestyle Changes Across Different Causes of Hypertension
Lifestyle modifications play a crucial role in managing high blood pressure, regardless of the underlying cause. Dietary changes, regular physical activity, and stress reduction techniques can significantly impact blood pressure levels and improve overall cardiovascular health. While the degree of improvement may vary depending on the specific cause of hypertension, these changes are beneficial across the board. For example, even in cases of secondary hypertension caused by kidney disease, adopting a low-sodium diet and managing stress can help control blood pressure and reduce the burden on the kidneys. Similarly, for primary hypertension (where no specific cause is identified), lifestyle changes form the cornerstone of initial management. These changes can often reduce the need for medication or lessen the required dosage.
Comparison of Medication Classes for High Blood Pressure
Several classes of medications are used to treat high blood pressure, each working through different mechanisms.
- Thiazide diuretics increase sodium and water excretion, reducing blood volume and lowering blood pressure. Potential side effects include dehydration, electrolyte imbalances, and increased blood sugar.
- ACE inhibitors block the production of angiotensin II, a potent vasoconstrictor. This leads to vasodilation and reduced blood pressure. Side effects can include a dry cough, dizziness, and kidney problems.
- Angiotensin receptor blockers (ARBs) similarly block angiotensin II but through a different mechanism, often being better tolerated by those who experience a cough with ACE inhibitors. Side effects are similar to ACE inhibitors, though often less frequent or severe.
- Beta-blockers reduce heart rate and contractility, lowering cardiac output and blood pressure. Common side effects include fatigue, bradycardia (slow heart rate), and bronchospasm (in individuals with asthma or COPD).
- Calcium channel blockers relax blood vessels by inhibiting calcium influx into vascular smooth muscle cells. Side effects can include headache, dizziness, and swelling in the ankles.
The choice of medication depends on factors such as the patient’s age, other health conditions, and the severity of hypertension. Often, a combination of medications is necessary to achieve optimal blood pressure control.
Decision-Making Flowchart for Treatment Strategies
The selection of appropriate treatment strategies is a multi-step process considering individual patient factors and the underlying cause of hypertension.
- Assess Blood Pressure: Measure blood pressure to confirm hypertension.
- Identify Underlying Cause: Investigate potential causes through physical examination, blood tests, and imaging studies.
- Lifestyle Modifications: Implement dietary changes, exercise program, stress management techniques.
- Monitor Blood Pressure: Regularly monitor blood pressure response to lifestyle changes.
- Medication Consideration: If lifestyle changes are insufficient, consider medication based on patient characteristics and identified cause. (Refer to the medication class comparison above).
- Medication Adjustment: Adjust medication dosage or combination based on ongoing blood pressure monitoring.
- Regular Follow-up: Schedule regular checkups to monitor blood pressure, assess medication effectiveness, and make adjustments as needed.
Designing a Personalized High Blood Pressure Management Plan
A personalized plan integrates lifestyle modifications and medical interventions, tailored to the individual’s specific needs and the underlying cause of their hypertension. This plan should be developed in collaboration with a healthcare professional.
For example, a patient with hypertension secondary to renal artery stenosis might require medication to manage blood pressure alongside interventional procedures to address the underlying stenosis. Conversely, a patient with primary hypertension might initially focus on lifestyle changes, with medication added only if blood pressure remains uncontrolled. The plan should include specific dietary guidelines, a structured exercise regimen, stress-reduction strategies (like yoga or meditation), regular blood pressure monitoring, and a schedule for medication intake (if prescribed).
Infographic on Healthy Lifestyle Choices
An informative infographic for blood pressure management would visually depict key lifestyle modifications. It would include sections on: a sample DASH diet meal plan emphasizing fruits, vegetables, whole grains, and lean protein; examples of moderate-intensity aerobic exercises (like brisk walking or cycling); stress-management techniques such as deep breathing exercises or mindfulness; and visual representations of recommended sodium intake and portion sizes. The infographic would highlight the positive impact of these lifestyle choices on blood pressure and overall health, reinforcing the importance of consistent adherence to the personalized management plan.
End of Discussion
Managing high blood pressure requires a multifaceted approach encompassing lifestyle modifications and, when necessary, medical intervention. By understanding the various causes and diagnostic procedures, individuals can proactively address their risk factors and work collaboratively with healthcare professionals to achieve optimal blood pressure control. Prioritizing regular checkups and adopting a healthy lifestyle are paramount in mitigating the long-term consequences of hypertension.