Hormonal imbalances affect millions, subtly disrupting daily life and overall well-being. Understanding the common symptoms and diagnostic pathways is crucial for effective treatment. This guide explores six prevalent hormone imbalances, detailing their unique symptoms, diagnostic tests, and interpretation of results, empowering individuals to navigate this complex area of health.
We’ll delve into the nuances of differentiating between these imbalances, examining how various symptoms can overlap and the importance of comprehensive testing. Through clear explanations and illustrative examples, we aim to demystify the diagnostic process, providing you with the knowledge to better understand your own hormonal health and advocate for effective care.
Recognizing Symptoms of Hormone Imbalances
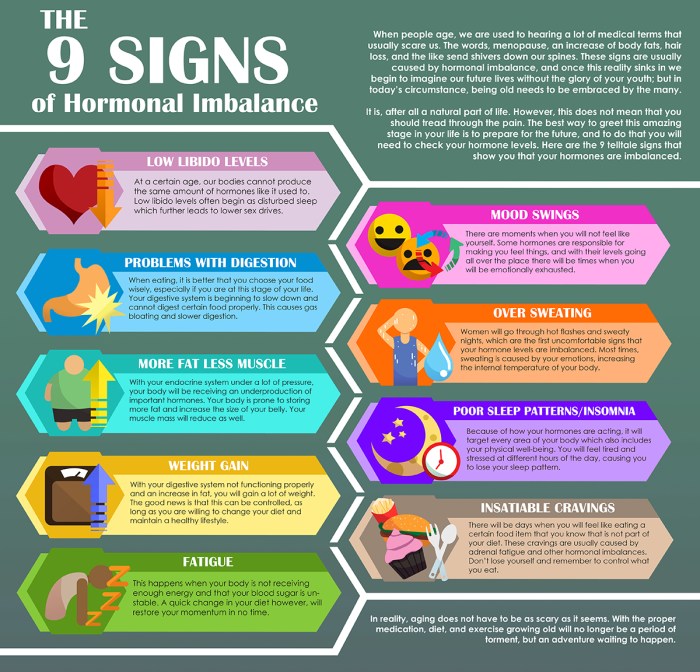
Recognizing the symptoms of hormone imbalances can be challenging because they often overlap and mimic other health conditions. Many symptoms are subtle and may develop gradually, making it difficult to pinpoint the underlying cause. Accurate diagnosis requires a thorough evaluation by a healthcare professional, considering individual medical history and conducting appropriate tests. The following information provides a general overview of common symptoms associated with six common hormone imbalances; however, it is not a substitute for professional medical advice.
Common Symptoms of Six Hormone Imbalances
Understanding the varied symptoms associated with different hormone imbalances is crucial for early detection and effective management. The following table summarizes key symptoms for each imbalance. Note that these are not exhaustive lists, and individuals may experience a different combination or severity of symptoms.
| Hormone Imbalance | Symptom 1 | Symptom 2 | Symptom 3 |
|---|---|---|---|
| Hypothyroidism (Underactive Thyroid) | Fatigue and lethargy | Weight gain despite dietary changes | Intolerance to cold |
| Hyperthyroidism (Overactive Thyroid) | Unexplained weight loss | Increased heart rate and palpitations | Anxiety and irritability |
| Insulin Resistance/Type 2 Diabetes | Increased thirst and frequent urination | Elevated blood sugar levels | Slow-healing wounds |
| Estrogen Dominance | Heavy or irregular menstrual bleeding | Breast tenderness | Weight gain around the hips and thighs |
| Testosterone Deficiency (in men) | Decreased libido | Erectile dysfunction | Fatigue and decreased muscle mass |
| Cortisol Imbalance (High or Low) | Chronic fatigue | Difficulty sleeping | Mood swings and irritability (high cortisol); feelings of depression and apathy (low cortisol) |
Distinguishing Between Hormone Imbalances
While symptom overlap exists, subtle differences can help distinguish between imbalances. For instance, weight gain is associated with hypothyroidism, but weight loss characterizes hyperthyroidism. Similarly, while both estrogen dominance and hypothyroidism can cause weight gain, estrogen dominance often manifests with specific weight gain patterns (hips and thighs), and menstrual irregularities are more prominent. Men with testosterone deficiency will present differently than women with estrogen dominance, showcasing symptoms directly related to sexual function and muscle mass. Cortisol imbalances, affecting stress response, present with fatigue but also distinct mood disturbances, differing in character depending on whether cortisol is high or low. Accurate diagnosis requires considering the complete symptom picture and utilizing appropriate laboratory tests.
Diagnostic Pathway Based on Symptoms
A flowchart illustrating the diagnostic pathway would begin with initial symptom presentation (e.g., fatigue, weight changes, menstrual irregularities). This would lead to a preliminary assessment by a healthcare professional, taking into account medical history and risk factors. Subsequent steps would involve targeted blood tests to measure relevant hormone levels (TSH, T3, T4 for thyroid; glucose and insulin for diabetes; estradiol, progesterone, testosterone as appropriate). Imaging studies or other specialized tests might be indicated depending on the initial findings. The diagnostic process is iterative, with results from initial tests guiding further investigations until a definitive diagnosis is reached. The flowchart would visually represent this iterative process, branching based on the results of each step. It is crucial to remember that this is a complex process and should only be undertaken under the guidance of a qualified healthcare professional.
Diagnostic Tests and Procedures for Hormone Imbalances
Diagnosing hormone imbalances requires a multifaceted approach, combining a thorough medical history, physical examination, and specific laboratory tests. The choice of tests depends on the suspected imbalance and the individual’s symptoms. Accurate diagnosis is crucial for effective treatment and management.
Several diagnostic tests are available to assess various hormone imbalances. These tests measure hormone levels in blood, urine, or saliva, providing valuable insights into endocrine function. The interpretation of results requires consideration of factors such as age, sex, and overall health. It’s important to remember that test results should be interpreted in conjunction with the patient’s clinical presentation and medical history.
Common Diagnostic Tests for Hormone Imbalances
The following bullet points Artikel common diagnostic tests used to evaluate six common hormone imbalances. These tests are not exhaustive, and other tests may be necessary depending on the specific clinical situation.
- Thyroid Hormones (Hypothyroidism & Hyperthyroidism): Thyroid Stimulating Hormone (TSH), Free Thyroxine (FT4), and Free Triiodothyronine (FT3) blood tests. TSH measures the pituitary gland’s signal to the thyroid. FT4 and FT3 measure the active thyroid hormones in the blood. High TSH with low FT4/FT3 indicates hypothyroidism; low TSH with high FT4/FT3 indicates hyperthyroidism. Thyroid ultrasound may also be used to assess thyroid size and structure.
- Insulin & Glucose (Insulin Resistance & Type 2 Diabetes): Fasting blood glucose (FBG) measures glucose levels after an overnight fast. Oral Glucose Tolerance Test (OGTT) measures glucose levels at intervals after consuming a sugary drink. HbA1c measures average blood glucose levels over the past 2-3 months. Insulin levels can be measured to assess insulin resistance. High FBG, abnormal OGTT, and elevated HbA1c indicate diabetes or prediabetes.
- Cortisol (Cushing’s Syndrome & Addison’s Disease): Salivary cortisol tests measure cortisol levels throughout the day to assess the body’s cortisol rhythm. 24-hour urine cortisol tests measure total cortisol excretion. Blood tests can measure cortisol levels at specific times. High cortisol levels suggest Cushing’s syndrome; low cortisol levels suggest Addison’s disease. Imaging studies (e.g., MRI) may be used to identify the cause of cortisol imbalance.
- Testosterone (Hypogonadism in Men): Total testosterone, free testosterone, and luteinizing hormone (LH) and follicle-stimulating hormone (FSH) blood tests are used. Low testosterone levels with elevated LH/FSH suggest primary hypogonadism (testicular failure); low testosterone with low LH/FSH suggests secondary hypogonadism (pituitary or hypothalamic dysfunction).
- Estrogen & Progesterone (Hormonal Imbalances in Women): Blood tests measure levels of estradiol (main estrogen), progesterone, and follicle-stimulating hormone (FSH) and luteinizing hormone (LH) throughout the menstrual cycle. These tests help evaluate ovulation, assess menstrual irregularities, and diagnose conditions like polycystic ovary syndrome (PCOS).
- Growth Hormone (Growth Hormone Deficiency & Excess): Growth hormone stimulation tests involve administering substances that stimulate GH release and measuring the response. Insulin-like growth factor 1 (IGF-1) blood tests assess the effects of GH. High IGF-1 suggests excess GH; low IGF-1 suggests GH deficiency. MRI of the pituitary gland may be needed to identify underlying causes.
Advantages and Disadvantages of Different Testing Methods
Different testing methods have varying advantages and disadvantages. For example, salivary cortisol testing is less invasive than blood tests, but may not reflect total cortisol production. OGTT is more comprehensive than FBG in assessing glucose metabolism but requires more time and preparation. Choosing the most appropriate test requires careful consideration of the clinical context and patient factors.
Hormone Levels, Implications, and Next Steps
The following table summarizes normal ranges, implications of abnormal results, and potential next steps in diagnosis for selected hormones. These ranges can vary slightly depending on the laboratory and testing method. It is crucial to consult with a healthcare professional for proper interpretation of results and guidance on next steps.
| Hormone | Normal Range (Example – May Vary) | Abnormal Range Implications | Next Steps |
|---|---|---|---|
| TSH | 0.4-4.0 µIU/mL | High: Hypothyroidism; Low: Hyperthyroidism | Further thyroid function tests (FT4, FT3), thyroid ultrasound, potentially thyroid biopsy |
| Fasting Blood Glucose (FBG) | 70-100 mg/dL | High: Diabetes or prediabetes | Oral Glucose Tolerance Test (OGTT), HbA1c, insulin testing |
| Cortisol (Morning) | 5-25 µg/dL | High: Cushing’s syndrome; Low: Addison’s disease | 24-hour urine cortisol, salivary cortisol testing, imaging studies (MRI) |
| Testosterone (Men) | 300-1000 ng/dL | Low: Hypogonadism | LH, FSH testing, further investigation of potential causes |
| Estradiol (Women, Follicular Phase) | 50-400 pg/mL | Low: Ovulatory dysfunction; High: Possible PCOS | Progesterone testing, LH/FSH testing, ultrasound |
| IGF-1 | Variable depending on age and sex | High: Acromegaly (excess growth hormone); Low: Growth hormone deficiency | Growth hormone stimulation tests, MRI of pituitary gland |
Interpreting Test Results and Differential Diagnosis

Interpreting hormone test results requires a nuanced understanding of normal ranges, potential interferences, and the interplay between different hormones. Simply observing values outside of a reference range isn’t sufficient for diagnosis; clinical context, patient history, and potentially additional testing are crucial. Confounding factors like stress, diet, medications, and the time of day when samples are taken can significantly influence results. A thorough differential diagnosis considers the possibility of multiple simultaneous imbalances.
Understanding Individual Hormone Test Results
Each hormone test has its own specific interpretation. For example, a low thyroid-stimulating hormone (TSH) level might indicate hyperthyroidism, but it could also be due to medication or pituitary dysfunction. Similarly, elevated cortisol levels could be indicative of Cushing’s syndrome, stress, or medication side effects. It is vital to consider the entire clinical picture rather than focusing on isolated results. A comprehensive interpretation integrates the results of multiple tests, alongside the patient’s symptoms and medical history.
Common Scenarios of Coexisting Hormone Imbalances
Frequently, hormone imbalances aren’t isolated events. For instance, hypothyroidism can lead to secondary imbalances in sex hormones, resulting in irregular periods or reduced libido in women, and decreased libido or erectile dysfunction in men. Similarly, insulin resistance, often associated with metabolic syndrome, can impact sex hormone production and contribute to conditions like polycystic ovary syndrome (PCOS). Another common scenario involves the interaction between cortisol and thyroid hormones. Chronic stress leading to high cortisol can suppress thyroid function, causing symptoms that overlap with both conditions. Differentiating between these requires careful evaluation of symptoms and the pattern of hormone test results.
Differential Diagnosis in Practice: A Hypothetical Case Study
Consider a 35-year-old woman presenting with fatigue, weight gain, irregular periods, and hair loss. Her initial blood tests reveal elevated TSH (indicative of hypothyroidism), elevated prolactin (a hormone potentially affected by hypothyroidism or other conditions), and slightly elevated cortisol levels. A simple interpretation might focus on the elevated TSH, diagnosing hypothyroidism. However, the elevated prolactin and cortisol levels suggest a more complex picture. Further investigation, perhaps including tests for adrenal function and an assessment of lifestyle factors, would be necessary to determine if the elevated cortisol is due to stress, a separate adrenal disorder, or a consequence of the hypothyroidism. The elevated prolactin might also warrant further investigation to rule out a pituitary adenoma. A comprehensive interpretation would consider the interaction of these hormones and guide treatment accordingly, perhaps involving thyroid hormone replacement and stress management techniques. Ignoring the other hormonal imbalances could lead to incomplete treatment and persistent symptoms.
Wrap-Up
Successfully navigating the diagnosis of hormone imbalances requires a multi-faceted approach. By understanding the common symptoms, utilizing appropriate diagnostic tests, and carefully interpreting the results, individuals can gain valuable insights into their hormonal health. This comprehensive understanding empowers informed discussions with healthcare professionals, leading to more effective management and improved overall well-being. Remember, early detection and intervention are key to successful outcomes.