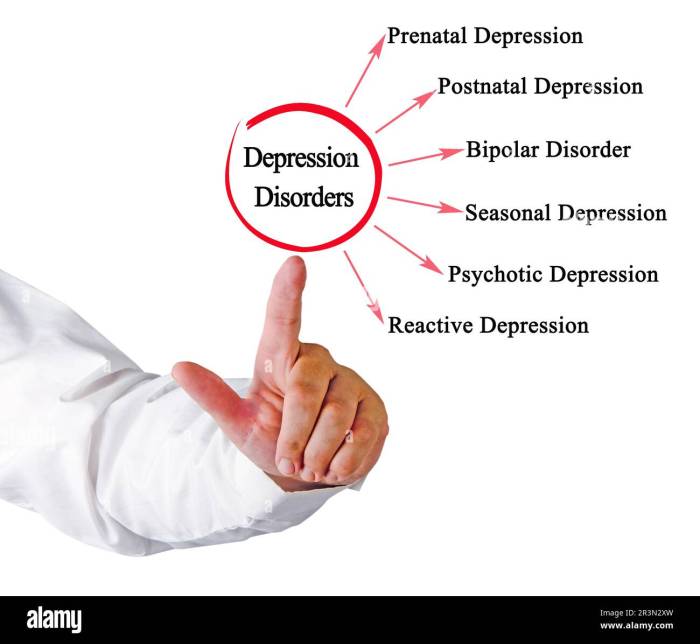
Understanding depression is crucial for effective treatment. This guide delves into six distinct types of depression, providing insights into their unique symptoms, diagnostic criteria, and the challenges in differentiating them. We’ll explore Major Depressive Disorder, Persistent Depressive Disorder, and the depressive aspects of Bipolar Disorder, highlighting key differences and similarities to aid in accurate identification and diagnosis.
By examining the nuances of each type, we aim to empower individuals and healthcare professionals with a clearer understanding of this complex mental health condition. This knowledge can lead to more timely and appropriate interventions, improving the lives of those affected by depression.
Major Depressive Disorder (MDD)
Major Depressive Disorder, often referred to as clinical depression, is a serious mood disorder characterized by persistent feelings of sadness, loss of interest, and a range of other debilitating symptoms. Understanding its diagnostic criteria and manifestations is crucial for effective treatment and support.
Diagnostic Criteria for MDD (DSM-5)
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), Artikels specific criteria for diagnosing MDD. A diagnosis requires the presence of at least five of the listed symptoms for at least two weeks, representing a change from previous functioning, and causing clinically significant distress or impairment in social, occupational, or other important areas of functioning. One of the symptoms must be either depressed mood or loss of interest or pleasure.
Common Symptoms of MDD
MDD presents a wide spectrum of symptoms, affecting both the body and the mind.
Physical Manifestations of MDD
Physical symptoms are often overlooked but can significantly impact daily life. These include changes in appetite or weight (either significant weight loss or gain), sleep disturbances (insomnia or hypersomnia), fatigue or loss of energy, psychomotor agitation or retardation (restlessness or slowed movements), and feelings of worthlessness or excessive guilt. These physical symptoms can exacerbate the emotional distress, creating a vicious cycle.
Emotional Manifestations of MDD
Emotional symptoms are central to MDD. These include persistent sadness, feelings of hopelessness and despair, loss of interest or pleasure in activities once enjoyed (anhedonia), difficulty concentrating, indecisiveness, and recurrent thoughts of death or suicide. The intensity and duration of these symptoms vary among individuals.
Impact of MDD on Daily Life
MDD significantly impacts various aspects of daily life. At work, it can lead to decreased productivity, absenteeism, and even job loss. Relationships suffer due to social withdrawal, irritability, and communication difficulties. Personal care, such as hygiene and self-care, is often neglected. Simple tasks that were once effortless become overwhelming and burdensome. For example, someone with MDD might find it impossible to get out of bed, shower, or prepare a meal, leading to further isolation and deterioration.
Comparison of MDD Symptoms with Other Depressive Disorders
| Symptom | Major Depressive Disorder (MDD) | Persistent Depressive Disorder (Dysthymia) | Bipolar Disorder (Depressive Episode) |
|---|---|---|---|
| Depressed Mood | Present for at least two weeks | Present for at least two years | Present during a depressive episode, often alternating with manic or hypomanic episodes |
| Loss of Interest/Pleasure | Present for at least two weeks | Present for at least two years | Present during a depressive episode |
| Sleep Disturbances | Insomnia or hypersomnia | Insomnia or hypersomnia | Insomnia or hypersomnia |
| Fatigue/Loss of Energy | Present | Present | Present |
Persistent Depressive Disorder (Dysthymia)

Persistent Depressive Disorder, also known as dysthymia, is a chronic type of depression characterized by a persistently low mood for a significantly longer duration than Major Depressive Disorder (MDD). Unlike MDD, which involves episodes of intense depressive symptoms, dysthymia presents with a more subdued but persistent low-grade depression that lasts for at least two years in adults. This chronic nature makes it a distinct and often challenging condition to diagnose and treat effectively.
Persistent Depressive Disorder shares some overlapping symptoms with MDD, but differs significantly in terms of duration and intensity. Both conditions involve symptoms like low mood, fatigue, and difficulty concentrating. However, MDD is characterized by more intense and debilitating symptoms that often interfere significantly with daily life, whereas dysthymia involves a less severe but persistent state of low mood. The crucial difference lies in the duration; MDD episodes are typically shorter and more episodic, while dysthymia is a continuous, long-term condition. This prolonged nature of dysthymia can lead to significant challenges in diagnosis and treatment.
Comparing and Contrasting MDD and Persistent Depressive Disorder Symptoms and Duration
MDD and Persistent Depressive Disorder (PDD) both involve symptoms such as sadness, loss of interest, sleep disturbances, and fatigue. However, the intensity and duration of these symptoms differ considerably. MDD is characterized by a period of at least two weeks of significantly depressed mood or loss of interest, accompanied by other symptoms such as changes in appetite or sleep, low energy, feelings of worthlessness, and difficulty concentrating. In contrast, PDD involves a persistently depressed mood for at least two years in adults (one year in children and adolescents), with symptoms being less severe than in MDD but persistent and pervasive. The key differentiator is the chronicity; MDD is episodic, while PDD is a continuous, low-grade depression. Someone with MDD might experience periods of relatively normal mood interspersed with episodes of intense depression, whereas someone with PDD experiences a consistently low mood, even if it fluctuates slightly in intensity.
Challenges in Diagnosing Persistent Depressive Disorder
The chronic nature of Persistent Depressive Disorder presents significant diagnostic challenges. Because the symptoms are less severe than in MDD, they may be overlooked or attributed to other factors, such as stress or personality traits. Individuals with PDD may become accustomed to their low mood, perceiving it as their “normal” state, making them less likely to seek help. Furthermore, the overlapping symptoms with other chronic conditions, such as anxiety disorders, chronic pain syndromes, and thyroid disorders, complicate the diagnostic process. Clinicians need to carefully assess the patient’s history, symptoms, and other relevant factors to accurately differentiate PDD from other conditions. The lack of clear diagnostic criteria and the subtle nature of the symptoms contribute to underdiagnosis and delayed treatment.
Differentiating Persistent Depressive Disorder from Other Chronic Health Conditions
Differentiating Persistent Depressive Disorder from other chronic conditions with overlapping symptoms requires a thorough clinical evaluation. For example, chronic fatigue syndrome (CFS) and fibromyalgia share symptoms such as fatigue, pain, and sleep disturbances with PDD. However, CFS is characterized by persistent, unexplained fatigue, while fibromyalgia involves widespread musculoskeletal pain. Similarly, anxiety disorders can present with symptoms like irritability, difficulty concentrating, and sleep problems, but anxiety is typically characterized by excessive worry and fear, whereas PDD is characterized by a pervasive low mood. A comprehensive assessment, including a detailed medical history, physical examination, and psychological evaluation, is crucial to accurately distinguish PDD from other chronic conditions.
Effective Treatment Approaches for Persistent Depressive Disorder
Effective treatment for Persistent Depressive Disorder often involves a combination of approaches tailored to the individual’s needs.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) is particularly effective in addressing negative thought patterns and behaviors associated with PDD. It helps individuals identify and challenge negative thoughts and develop coping mechanisms to manage their symptoms.
- Medication: Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can be helpful in alleviating depressive symptoms. The choice of medication and dosage will depend on individual factors.
- Lifestyle Modifications: Regular exercise, a healthy diet, sufficient sleep, and stress management techniques are crucial components of effective treatment. These lifestyle changes can significantly improve mood and overall well-being.
- Other Therapies: Other therapeutic approaches, such as interpersonal therapy and mindfulness-based therapies, may also be beneficial for some individuals with PDD.
Bipolar Disorder (with Depressive Episodes)

Bipolar disorder is a mental illness characterized by extreme shifts in mood, energy, and activity levels. Unlike Major Depressive Disorder, which primarily involves persistent low mood, bipolar disorder involves both depressive episodes and periods of elevated mood, known as manic or hypomanic episodes. Understanding the differences between these mood states is crucial for accurate diagnosis and treatment.
Depressive Episodes in Bipolar Disorder versus MDD
Depressive episodes in bipolar disorder share many symptoms with Major Depressive Disorder (MDD), including persistent sadness, loss of interest, sleep disturbances, fatigue, and changes in appetite. However, a key distinction lies in the context of these symptoms. In bipolar disorder, depressive episodes occur in the context of a history of manic or hypomanic episodes, which are absent in MDD. The severity and duration of depressive episodes can also vary between the two disorders. For instance, depressive episodes in bipolar disorder may be more intense or last longer than those seen in MDD. Furthermore, the response to treatment may also differ.
The Role of Manic or Hypomanic Episodes in Bipolar Disorder Diagnosis
Manic and hypomanic episodes are defining features of bipolar disorder. Manic episodes involve a distinct period of abnormally and persistently elevated, expansive, or irritable mood, lasting at least one week. This elevated mood is accompanied by increased energy, racing thoughts, impulsive behavior, decreased need for sleep, and potentially delusional thinking or grandiosity. Hypomanic episodes share similar symptoms but are less severe and do not significantly impair daily functioning or require hospitalization. The presence of these episodes, even if they are interspersed with periods of normal mood, is essential for differentiating bipolar disorder from MDD, where such episodes are absent. A history of these episodes, even if not currently experienced, significantly contributes to the diagnosis.
Distinguishing Between Bipolar I and Bipolar II Disorders
The distinction between Bipolar I and Bipolar II disorders hinges primarily on the severity and type of mood episodes experienced. Bipolar I disorder is characterized by at least one manic episode, which may or may not be preceded or followed by depressive episodes. Bipolar II disorder, on the other hand, is defined by at least one hypomanic episode and at least one major depressive episode. Crucially, individuals with Bipolar II disorder have never experienced a full-blown manic episode. While both disorders involve depressive symptoms, the presence or absence of a manic episode is the key differentiator. The depressive symptoms themselves might be very similar in both conditions, making accurate diagnosis dependent on the careful evaluation of the entire mood history.
Diagnostic Flowchart for Bipolar Disorder
The following flowchart illustrates the diagnostic process for bipolar disorders, focusing on the role of depressive symptoms within the broader context of mood episodes:
| Start | |
|---|---|
| History of elevated mood (manic or hypomanic)? | Yes –> Go to Bipolar I/II differentiation; No –> Consider other diagnoses (e.g., MDD) |
| Severity of elevated mood? | Full manic episode (at least one week) –> Bipolar I; Hypomanic episode (at least four days) –> Bipolar II |
| Presence of depressive episodes? | Yes –> Diagnose Bipolar I or Bipolar II based on the previous step; No –> Requires further evaluation to rule out other diagnoses |
| End |
Final Wrap-Up

Successfully navigating the complexities of depression requires a multifaceted approach. This guide has provided a framework for understanding six key types, emphasizing the importance of professional diagnosis and tailored treatment plans. Remember, seeking help is a sign of strength, and with the right support, recovery is possible. Further research and ongoing dialogue with healthcare professionals are vital for managing depression effectively.